A Hospital in Ballina to European Standards.

This report presents a preliminary appraisal of the proposed establishment of a new hospital facility in Ballina, Mayo. The aim of this project is to address the existing healthcare gap in the region and provide essential medical services to a population of approximately 35,000 within a 30 km radius. By benchmarking against best-in-class public healthcare systems and drawing insights from similar-sized hospitals in countries like Canada, the Scandinavian countries, and parts of Western Europe, we have identified the key services and specialties that can be reasonably expected in a hospital of this scale.
The proposed hospital will offer a comprehensive range of services, including emergency care, inpatient care, diagnostic services, surgical services, outpatient clinics, specialized services, pharmacy services, support services, telemedicine facilities, and community outreach and health promotion initiatives. By providing these services locally, the hospital will significantly reduce the need for residents to travel long distances for medical care, improving accessibility and convenience for the community.
Market Analysis:
The market analysis indicates a strong demand for a new hospital facility in Ballina. The current healthcare infrastructure in the area is insufficient to meet the growing needs of the population. By establishing a new hospital, we can cater to the increasing demand for healthcare services and alleviate the burden on existing facilities.
Furthermore, the proximity of Ballina to other towns and villages in Mayo County makes it an ideal location for a regional healthcare hub. This will not only benefit the local population but also attract patients from surrounding areas, boosting the economic growth of the region.
Financial Viability:
The financial viability of the proposed hospital facility is promising. Through a comparative cost analysis, we have determined that the initial investment required for construction, equipment, and staffing can be recovered within a reasonable timeframe when offset against the direct an indirect economic benefits.
Benefits to the Community:
The establishment of a new hospital facility in Ballina will bring numerous benefits to the community. Firstly, it will create job opportunities for healthcare professionals, supporting local employment and economic development. Secondly, it will enhance the overall quality of healthcare services available, ensuring that residents receive timely and efficient medical care. This will lead to improved health outcomes, reduced waiting times, and increased patient satisfaction.
Conclusion:
In conclusion, the establishment of a new hospital facility in Ballina, Mayo, holds great promise for the community. By addressing the existing healthcare gap, improving accessibility, and providing a comprehensive range of services, the proposed hospital will significantly enhance the quality of healthcare in the region. With its strong financial viability and numerous benefits to the community, we are confident in the success of this project. We recommend moving forward with the necessary steps to bring this vision to reality, ensuring a brighter and healthier future for the residents of Ballina and its surrounding areas.
Policy Background
Regional hospitals and public healthcare in general has been gradually downgraded since the budget cuts of the 1980s, losing even the most basic facilities, for example maternity care, or even closing altogether. The economic challenges and spending cuts in Ireland during the 1980s were influenced by a combination of domestic factors and broader international economic trends, including the rise of neoliberal economic doctrine advocating public spending cuts and privatization of previously free services. The country also faced high unemployment rates, emigration, public debt, and other economic problems during this period.
The decline was exacerbated from the 2000s with the reconfiguration of hospital services in Ireland, including the downgrading of some regional hospitals and centralization of most services. The main reasons cited for these changes were to enhance patient safety, improve the quality of care, and make better use of resources.
Here’s a brief overview of the timeline of changes:
Report of the National Acute Services Review Group (2001): This report recommended a networked approach to delivering hospital services. The idea was that not every hospital would provide all services. By centralizing complex and specialist services in larger hospitals, the health service could ensure a high volume of cases, which is often associated with better outcomes.
Quality and Fairness: A Health System for You (2001): This national health strategy emphasized patient safety and quality of care. It highlighted the need for some services to be provided in high-volume centers where specialist teams could maintain and develop their skills.
The Hanly Report (2003): Formally known as “The Report of the National Task Force on Medical Staffing,” it highlighted the importance of having a critical mass of cases to maintain clinical skills, especially in areas like surgery. As a result, it recommended the reconfiguration of certain services. This report became particularly controversial when it came to the downgrading of some regional hospitals, with concerns about longer travel times for patients and the impact on local communities.
Micheál Martin established the HSE in the Health Act 2004 and it officially began its operations on January 1, 2005 which centralized all decision making in Dublin, ending regional governance of healthcare. Over the years, there have been criticisms of the HSE related to bureaucracy, service delivery, and other issues. Various reforms and changes have been proposed and implemented since its inception to address these concerns and improve the health service delivery system in Ireland but with limited, if any, success.
Smaller Hospitals Framework (2013): This document clarified the role of smaller hospitals and aimed to ensure they are a vital part of the healthcare system. It proposed that smaller hospitals could still deliver a significant amount of care but highlighted that certain complex cases should be treated in larger hospitals.
Safety Concerns: In certain cases, concerns about patient safety due to inadequate resources or staffing might have led to the decision to centralize services. For example, maternity units might be centralized to ensure they can provide 24/7 emergency obstetric and neonatal care.
Economic and Efficiency Reasons: Maintaining a full range of services in every hospital can be expensive and may not be the most efficient use of resources. Centralizing some services can allow for better use of specialist equipment and expertise.
These changes have been controversial. Many communities and advocacy groups have expressed concerns about longer travel times, reduced accessibility to care, and the economic impact on local areas when a hospital is downgraded or closed. The debates surrounding these decisions proposed a trade-off between providing the best possible care for patients and ensuring accessibility and fairness. In the context of the continuing poor performance of public healthcare in Ireland when benchmarked against its peers (as evidenced in the shockingly high take-up of private health insurance, almost half the adult population currently) this putative trade-off appears to have little if any credibility in practice.
The Proposal
Topography and Demographics: Ballina hospital has a hinterland taking in historical lands of Tír Amhlaidh and Gaileanga in Mayo and Tír Fhiachrach in Sligo. According to the 2016 census the population for the Municipal District on the towns’ western shore (Ballina MD) was 32,688 and on the eastern side (Ballymote - Tobercurry MD) 26,731. The Sligo MD is extremely large and mostly located outside the natural hinterland of Ballina so the portion attributable to it must be revised down accordingly. Without accurate figures to hand it can be reasonably argued that the target population for the hospital would be in the region of 35,000 - 40,000 people. It should be noted that the population has likely increased significantly since 2016. It must also be observed that the population is abnormally low by European standards and thus likely to grow exponentially when the policy deficiencies currently suppressing economic development in the area are finally addressed (lack of adequate Healthcare facilities being one of them).
The Hospital:
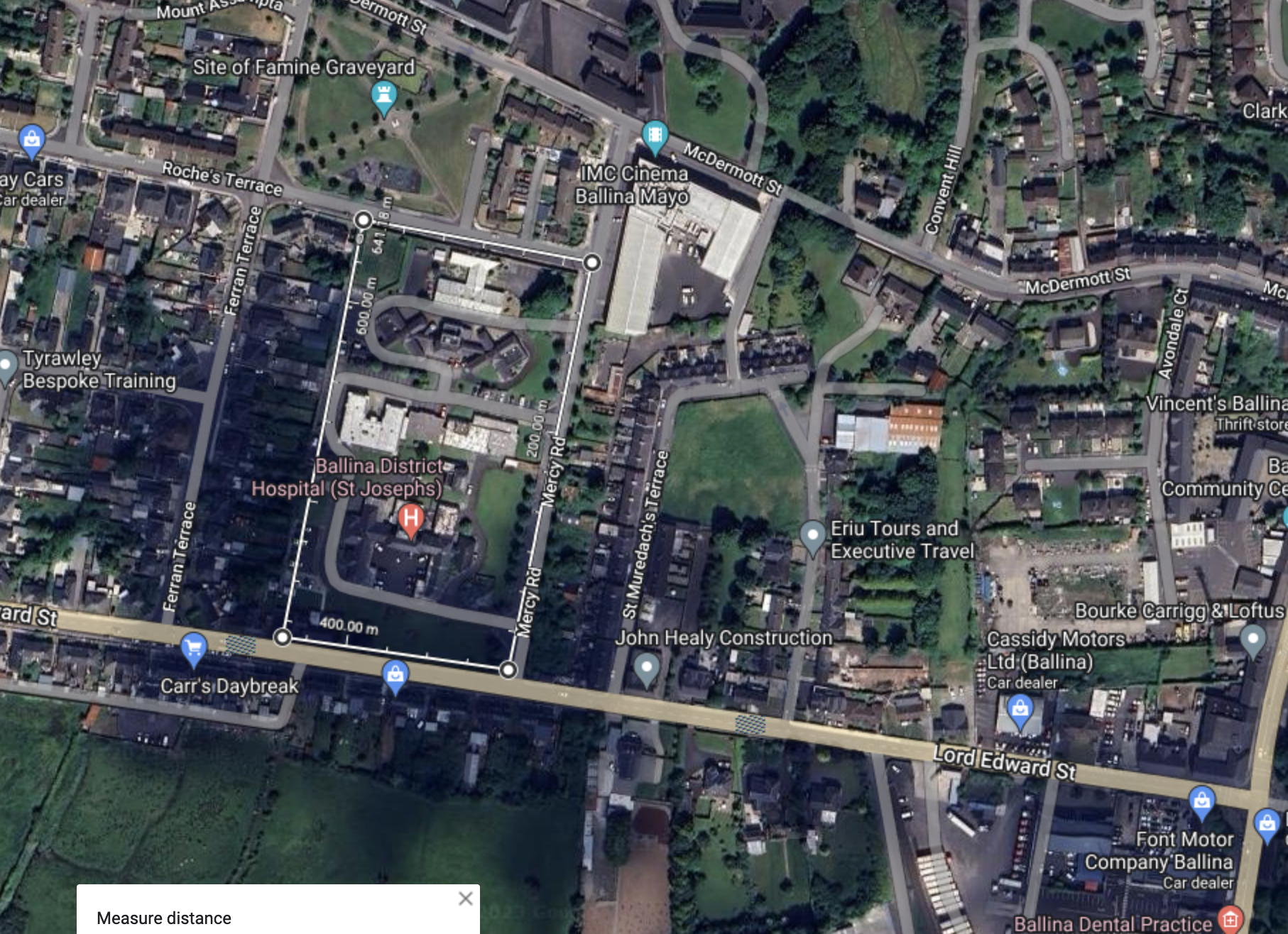
The current hospital, St. Joseph’s District Hospital, is located about a kilometer to the west of the central district of Ballina on a large rectangular site of approximately 20,000 square meters.
There are few detail as to what services the hospital currently offers, it is simply listed as providing “Acute and Community” services. There is no website or other information about the hospital readily available online.
The proposed project entails the establishment of a new ‘midi’ size hospital on the site, with appropriate service level based on European best practices. This will fill the current gap in healthcare provision and relieve the two regional hospitals, Castlebar and Sligo that currently service the region, as both face consistent overcrowding and are located too far away to provide adequate health care.
Proposed service spec
The upgrade of the current hospital is based on benchmarks from countries with best-in-class public healthcare. The following are some general services and specialties that a hospital serving a population of approximately 35,000 might provide. These services are often seen in similar-sized hospitals across countries like Canada, the Scandinavian countries (Norway, Sweden, Denmark, Finland), and parts of Western Europe (France, Spain, Italy):
- Emergency Department (ED):
- 24/7 access for acute and emergency care.
- On-call physicians for major specialties.
- Ambulance services connected with the hospital for immediate patient transport.
- Inpatient Care:
- Medical wards for general medicine.
- Surgical wards for general surgeries.
- Obstetric and gynecological ward for childbirth and women’s health.
- Pediatric ward for children’s health.
- Diagnostic Services:
- Laboratory services for blood and other biological sample testing.
- Radiology services, including X-ray, ultrasound, CT scan, and possibly MRI.
- Surgical Services:
- General surgery.
- Orthopedic surgery.
- Minor ENT (Ear, Nose, and Throat) procedures.
- Obstetric and gynecological surgeries.
- Some places might also have limited capabilities for urological and ophthalmological surgeries.
- Outpatient Clinics:
- General medicine.
- General surgery consultation.
- Obstetrics and gynecology.
- Pediatrics.
- Orthopedics.
- Chronic disease management clinics (e.g., diabetes, hypertension).
- Specialized Services:
- Physiotherapy and rehabilitation.
- Mental health and counseling services.
- Nutrition and dietary services.
- Pharmacy:
- Providing medicines for inpatients and outpatients.
- Medication counseling.
- Support Services:
- Hospital administration.
- Medical records.
- Maintenance and housekeeping.
- Telemedicine:
- For more specialized services that might not be available locally, a hospital might have telemedicine facilities to consult specialists in larger hospitals.
- Community Outreach and Health Promotion:
- Health education and promotion initiatives.
- Vaccination campaigns.
- Screening programs (e.g., for cancers, diabetes, etc.)
France case study
Given the geographical context and the size of the proposed hospital, the French healthcare system provides an excellent example to work from, indeed it is often rated as one of the best in the world. They have an extensive network of hospitals, ranging from smaller local hospitals to large university hospitals. Their system distinguishes hospitals into three main categories:
CHU (Centre Hospitalier Universitaire): Large teaching hospitals located in major cities, equipped with comprehensive and specialized medical services and attached to a medical university.
CHR (Centre Hospitalier Régional): Regional hospitals equipped to handle most medical issues. They provide general care and some specialized services but might not have super-specialized departments like organ transplantation, rare disease centers, etc.
CHG (Centre Hospitalier Général) or ‘Midi’ Hospitals: Smaller general hospitals serving smaller towns and rural areas. They provide essential care to local populations and are the type you seem to be referencing.
For a ‘Midi’ size hospital or a CHG in France, here is a typical template of services provided:
- Emergency Department: Open 24/7 for general emergencies and trauma.
- General Medicine and Surgery Wards: For the care of inpatients with general medical or surgical needs.
- Maternity Ward: Basic obstetric and gynecological care, including childbirth. Complicated cases may be referred to larger hospitals.
- Pediatric Ward: For general children’s health issues.
- Diagnostic Services: Including laboratory and standard radiology services.
- Outpatient Clinics: Day clinics for various specialties based on local needs.
- Rehabilitation: For patients recovering from surgeries, strokes, or other illnesses.
- Elderly Care: Depending on the demographics, some CHGs also have a unit dedicated to geriatric care.
- Short-Stay Surgery: For minor surgeries that don’t require extended hospitalization.
- Ambulatory Care: Treatment services that don’t require an overnight stay.
- Telemedicine Facilities: Given their more remote nature, CHGs have been integrating telemedicine facilities, particularly for specialities not present on-site.
Given Ballina hospital’s proximity to other facilities (~50 km away), it’s crucial for the local hospital to have a robust stabilization and referral system. The hospital should be equipped to stabilize patients in emergency situations and then safely transfer them to a larger hospital if specialized care is needed.
Further Recommended Study: 1. Site visit to a French CHG: Directly experiencing or understanding their operations would give the best insights. 2. Engage with French Healthcare Consultants: They can provide detailed operational insights and help customize a template for your specific region.
CHG spec, deeper dive.
A Centre Hospitalier Général (CHG) in France is designed to serve a comprehensive set of medical needs for its local population. However, it may not have every super-specialized service that a major university hospital might have. Here’s a list of specialist consultancy services typically available at a CHG:
- Cardiology: Diagnosis and treatment of heart-related diseases.
- Dermatology: Skin-related conditions and diseases.
- Endocrinology: Disorders of the endocrine system, including diabetes and thyroid diseases.
- ENT (Ear, Nose, and Throat): Otorhinolaryngology services.
- Gastroenterology: Digestive system and its disorders.
- General Surgery: Common surgical procedures including hernia repairs, appendectomies, etc.
- Geriatrics: Elderly care.
- Gynecology and Obstetrics: Women’s reproductive health, childbirth, etc.
- Hematology: Blood-related disorders.
- Internal Medicine: General internal conditions, often serving as a point of initial diagnosis and referral to other specialties.
- Nephrology: Kidney-related conditions.
- Neurology: Nervous system and its disorders.
- Orthopedics: Bone, joint, and muscle conditions.
- Pediatrics: Child health.
- Psychiatry: Mental health services.
- Pulmonology: Lung and respiratory conditions.
- Rheumatology: Joint and autoimmune disorders.
- Urology: Urinary system disorders and male reproductive system.
Staffing levels: This would largely vary based on the size of the facility, services offered, and local healthcare practices. However, as a heuristic for a CHG serving a population of around 35,000:
- Doctors: At least one specialist for each of the aforementioned specialties. This may mean a staff of 15-25 doctors, considering some specialties may have more than one consultant due to demand.
- Nursing staff: The number can vary widely based on the departments and the number of beds, but a rough heuristic might be 2-3 times the number of doctors, so around 30-75 nurses.
- Allied Health Professionals (like physiotherapists, radiographers, pharmacists, etc.): This number is harder to generalize but may range from 10-30.
- Administrative and support staff: This would include clerical workers, cleaners, facility management, etc., and might range from 20-50.
- Diagnostic and Laboratory Technicians: Depending on the services offered, 5-20.
- Ancillary and other staff: Kitchen, security, transport, etc., could range from 10-30.
Examples of CHG hospitals:
- Centre Hospitalier de Digne-les-Bains: Located in the Alpes-de-Haute-Provence department, Digne-les-Bains is a smaller city with a hospital that serves the surrounding area.
- Centre Hospitalier de Sarlat: Located in the Dordogne department, Sarlat is a small town with a hospital that serves both the town and its surrounding communes.
- Centre Hospitalier de Mont-de-Marsan: Located in the Landes department, while Mont-de-Marsan is a bit larger, its hospital might still provide a template for the kind of services a CHG offers to a population in your range.
- Centre Hospitalier de Millau: In the Aveyron department, Millau is a relatively small town with a hospital serving its local population.
- Centre Hospitalier de Bar-le-Duc: Located in the Meuse department, Bar-le-Duc has a hospital serving the needs of its local and surrounding community.
- Centre Hospitalier de Lourdes: Lourdes, in the Hautes-Pyrénées department, is an interesting case because, in addition to its local population, the town also caters to a large number of religious pilgrims every year. However, the core services of the hospital might still align with a CHG serving a typical local population.
Centre Hospitalier Jean LeClaire in the town of Sarlat. Sarlat-la-Canéda has a lower population than present day Ballina


Economic analysis of Proposal
Approximate operating cost per annum in euro: Estimating the operating cost for a CHG or similar hospital serving a population of around 35,000 in a Western European context is indeed a complex task. Costs can vary based on several factors, including the hospital’s geographical location, available services, patient volume, staffing levels, and more. Here’s a broad approach:
- Cost Per Bed Per Day: According to several reports, the average cost per hospital bed day across several Western European countries is somewhere between €400 to €1,000, with countries like France often being around the middle of this range. Let’s take an average value of €600 per bed day.
- Bed Utilization: Assuming an 85% bed occupancy rate over the year:
- Annual Cost: cost per day * 365 days
- Additional Costs: The above only considers direct costs associated with patient care. Hospitals also have administrative costs, equipment costs, maintenance, utilities, staff training, research (if applicable), and more. Adding an overhead of about 30% (see note)
Note on Maintenance, fixtures, wear and tear: The 30% overhead on top of direct patient care costs is intended to cover administrative costs, utilities, and other overheads. Howeve ongoing infrastructure maintenance, fixture replacements, and addressing wear and tear might not be fully encapsulated:
- Infrastructure Maintenance: Maintenance costs can often be about 2-4% of the building’s initial construction cost annually, depending on the age and condition of the facility.
- Equipment Maintenance and Replacement: Medical equipment, depending on its nature and usage, can have maintenance costs ranging from 5% to 10% of the equipment’s purchase price annually. In addition, some equipment needs to be periodically replaced.
- Fixtures and Wear & Tear: Replacing fixtures and addressing general wear and tear might consume another 1-2% of the hospital’s annual budget, depending on the age of the facility and the intensity of its usage.
Heuristics for beds per head of the population: This can vary by country and region. The number of beds a hospital should have can be influenced by several factors, including local health needs, the range of services offered, average length of stay, and hospital admission rates.
As of 2021, France had approximately 6 hospital beds per 1,000 inhabitants. This ratio combines all types of hospital beds, including those in CHUs, CHRs, and CHGs. For a population of 35,000, using this heuristic: 6 beds/1,000 inhabitants * 35 = 210 beds for 35,000 inhabitants.
However, it’s worth noting a few things:
- Specialization: Not all beds are general beds; this number would include specialized beds (intensive care, maternity, rehabilitation, etc.). The specific needs of your community would help determine the necessary breakdown.
- Proximity to Other Facilities: If there are other healthcare facilities nearby, especially larger hospitals, it’s possible that some of the healthcare needs of the local population are being addressed there. This might reduce the required number of beds at your local CHG.
- Shift Towards Outpatient Care: Over the years, there has been a global shift towards outpatient care due to advancements in medical procedures and a focus on preventive care. This trend reduces the need for inpatient beds.
- Local Health Needs: If the community has a higher proportion of elderly individuals or other specific health needs, it might require more beds.
Given these considerations, while the heuristic suggests around 210 beds for 35,000 people, in a practical setting and considering modern healthcare trends, a number like 100-150 might be more reasonable for a CHG, especially if there are other healthcare facilities within a reasonable distance.
Estimate of cost A ballpark operating cost based on the bed estimate and consider screening facilities can be estimated as follows:
- Bed Utilization:
- Let’s consider the midpoint of 100-150, which is 125 beds.
- Assuming an 85% bed occupancy rate over the year:
- 125 beds * 0.85 occupancy rate = 106.25 beds occupied on average each day.
- 106.25 beds * €600 = €63,750 per day.
- Annual Cost:
- €63,750 per day * 365 days = €23,268,750.
- Screening and Outpatient Services:
- Outpatient and screening facilities often operate differently in terms of costs when compared to inpatient services.
- If we assume that outpatient services and screening facilities (including imaging, lab work, preventive screenings, etc.) add an additional 15% to the total inpatient costs:
- €23,268,750 * 0.15 = €3,490,312.50.
- Total Direct Patient Care Costs:
- €23,268,750 (inpatient) + €3,490,312.50 (outpatient) = €26,759,062.50.
- Additional Costs:
- As before, adding a 30% overhead for administrative costs, utilities, equipment and infrastructure maintenance, fixtures, wear and tear, and other overheads:
- €26,759,062.50 * 1.30 = €34,787,781.25.
The ballpark annual operating cost, considering 125 beds and including screening facilities, would be approximately €34.8 million. The Cost Per Head Per Annum is €34,787,781.25 / 35,000 = €994.22. So, with the updated bed estimate and including screening facilities, the rough cost per head per annum would be just under €1,000. This would work out much cheaper than annual private insurance for the majority of citizens.
Economic benefits: What are the economic benefits for the local economy of funding this hospital overall?
- Direct Employment: Hospitals are significant employers. Not just medical staff, but also administrative staff, maintenance crews, and other support roles.
- Assume a conservative estimate that for every bed there are 5 employees (doctors, nurses, technicians, administrative staff, etc.). For 125 beds, that’s 625 jobs.
- Additionally, there’s indirect employment like suppliers, transportation, and other services linked to hospital functions.
- Local Businesses Boost: Hospital employees will patronize local businesses, such as cafes, restaurants, and shops, boosting the local economy. The influx of patients and their families might also provide additional business.
- Property Values: Typically, areas with good healthcare facilities see a rise in property values. Residents and potential homebuyers appreciate proximity to health facilities.
- Reduced Work Absenteeism: With better healthcare, timely screening, and local treatment facilities, residents won’t need to take as many days off work, leading to increased productivity.
- Economic Multiplier Effect: Money spent in the local economy cycles through it. For instance, a hospital worker spends their salary in a local shop, and then the shop owner spends that money, and so on. The multiplier effect in healthcare can vary, but let’s conservatively estimate it to be 1.5 for our purposes.
- So, €34.8 million * 1.5 = €52.2 million infused into the local economy annually.
- Attracting More Professionals: The presence of a hospital can draw other professionals into the area, possibly creating a hub for other health-related services, clinics, and establishments.
- Potential for Medical Tourism: Depending on the services offered and the reputation of the hospital, there could be opportunities to attract patients from outside the immediate catchment area.
- Increased Social Wellbeing: With better health outcomes, there’s likely to be increased life expectancy, reduced long-term illness, and a generally happier population, which can indirectly boost the economy.
Estimated Operating Benefit (Cost): Operating Costs: -€34.8 million Economic Benefits (Multiplier Effect): +€52.2 million Direct Employment Benefits (assuming an average wage of €30,000): +€18.75 million (625 jobs * €30,000) Net Gain: +€36.15 million
So, if we use a conservative economic multiplier effect and consider only the direct employment benefits, the introduction of the hospital could lead to a net positive economic flow of approximately €36.15 million annually, even after offsetting the operating costs.
Capital costs
The cost to construct a hospital can vary widely based on factors such as location, labor costs, materials, land acquisition costs, regulatory requirements, equipment costs, design, and the specific services to be offered. That said, let’s try to provide some context for constructing a minimum viable hospital for a community of 35,000 people.
- Construction Costs: As a rough ballpark, based on global averages, hospital construction can range from €2,000 to €5,000 per square meter (or more, depending on the factors mentioned). This figure can fluctuate significantly based on where in the world the construction is happening.
- For a mid-sized community hospital of, say, 10,000 square meters, the construction cost can range from:
- €20 million (at €2,000 per sq. m.) to
- €50 million (at €5,000 per sq. m.).
- Equipment Costs: These can vary based on the services the hospital plans to offer, but major costs will come from imaging equipment (MRI, CT scanners), laboratory equipment, surgical suites, and IT infrastructure. These can range from a few million euros to over €20 million for a hospital of the size you’re considering.
- Fit-Out and Ancillary Services: This includes furnishing, setting up patient rooms, offices, dining areas, and other hospital facilities. For a hospital of the size we’re discussing, this can add an additional €5-10 million.
Considering the above, a minimum viable hospital for a population of 35,000 could have an initial capital expenditure ranging from €30 million to €80 million or more.
Repurposing Extant Services: Repurposing existing buildings or facilities can save costs, but there are several things to consider:
- Structural Suitability: Hospitals have unique requirements, from larger elevator sizes to specific ventilation systems. The existing building should be structurally suited or adaptable to these needs.
- Location: The site should be easily accessible to the public, have good transport links, and ideally be centrally located within the served community.
- Size and Layout: The building should have enough space and an appropriate layout to house all necessary services, including patient rooms, operation theaters, labs, and more.
- Regulatory Requirements: There might be specific codes and standards that hospitals need to meet in your jurisdiction, and repurposed buildings must comply.
- Cost Analysis: Sometimes, repurposing can be more expensive than constructing a new building, especially if extensive modifications are required. A detailed cost-benefit analysis comparing new construction vs. renovation would be crucial.
- Desirability: From a community perspective, repurposing an iconic or cherished local building could face resistance, while other times, it might be seen as a way to breathe new life into a historic structure.
If there’s an appropriate existing structure available, refurbishing it can also be considered a viable option, perhaps reducing overall capital cost.
Cost-Benefit Analysis for a New Hospital:
Environmental Benefit: Reduction in private car roundtrips is also a significant factor to consider, let’s try to calculate the economic savings from this reduced travel:
- Estimate the Number of Trips Saved:
- Let’s make a conservative estimate. Assume out of the 35,000 population, 10% need to visit the hospital annually for services they’d otherwise have to travel for. That’s 3,500 patients.
- Now, assume each of those patients would make an average of 3 trips a year to the farther hospital. That’s a total of 10,500 trips annually.
- Calculate Distance Saved per Trip:
- Previously: 50 km roundtrip
- Now: 10 km roundtrip (since most will live within 5km of the new hospital)
- Distance saved per trip: 40 km So, annually, the total distance saved is 10,500 trips x 40 km = 420,000 km.
- Other Economic Benefits:
- Reduced wear and tear on vehicles, which translates into less frequent repairs and maintenance.
- Savings on time, which has an economic value, especially if patients or family members need to take time off work.
- Reduced traffic on roads, leading to lesser road maintenance costs.
Positive effect on Regional Healthcare: Certainly, introducing a new hospital to serve a local population of around 35,000 that currently relies on regional hospitals like Castlebar and Sligo will have multiple implications for these existing facilities. Here’s how such a development could impact the regional hospitals:
- Reduction in Patient Load:
- One of the most immediate benefits would be the reduction in the number of patients seeking services at Castlebar and Sligo from the 35,000 population that the new hospital serves. This would particularly ease the pressure on outpatient services, emergency departments, and routine surgical procedures.
- Decreased Overcrowding:
- Overcrowding is a significant stressor for hospitals. It can lead to increased waiting times, stressed medical staff, patient dissatisfaction, and even compromises in the quality of care. By diverting a portion of the patient population to the new hospital, Castlebar and Sligo might experience a relief in overcrowding issues, leading to better patient care.
- Specialization and Referral Systems:
- With the establishment of a new hospital, the existing regional hospitals could further specialize in specific services, knowing that general and routine medical needs are being handled by the new facility. This might lead to a more efficient healthcare ecosystem where each hospital plays to its strengths.
- Economic Impacts:
- With reduced patient loads, they might also be able to manage their resources better, potentially leading to cost savings.
- The reduction in patient numbers might also have an impact on staffing and resource allocation at the regional hospitals. This could lead to potential staff reallocations, reduced need for temporary staff, or the redirection of staff to other high-priority areas.
- Improved Patient Outcomes:
- Reduced overcrowding, shorter wait times, and more focused care (owing to possible specialization) can lead to improved patient outcomes. This will be beneficial for the reputation of the regional hospitals.
- Enhanced Staff Well-being:
- Overcrowded hospitals can be stressful work environments for healthcare professionals. Reducing the patient load can help in improving the work-life balance for the staff, reducing burnout, and potentially improving job satisfaction.
- Potential for Collaborative Efforts:
- The new hospital could collaborate with the regional hospitals for training, resource sharing, research, and specialized care. This can foster a sense of community and shared purpose among healthcare providers in the region.
- Infrastructure and Resource Reallocation:
- With the decreased pressure, the regional hospitals might find opportunities to renovate or repurpose areas of the hospital, upgrade equipment, or reallocate beds and resources to specialties that might have been previously underserved.
Economic Benefits estimate:
- Local economic boost: €52.2 million annually.
- Environmental savings: Let’s assume a conservative environmental savings (in terms of avoided fines, reduced healthcare costs due to better air quality, and other related factors) of €2 million annually.
- Savings to neighboring hospitals: Reduced patient loads might mean fewer complications from overcrowding, more efficient operations, and better patient outcomes. Let’s conservatively estimate a saving of €5 million annually.
- Healthier workdays/saved lives: This is tricky without detailed epidemiological data. However, for our model, let’s estimate the combined economic benefits of healthier workdays and saved lives at €10 million annually.
This totals an additional benefit of €69.2 million annually.
Net Present Value (NPV) Calculation Over 20 Years: Given the total benefits (direct economic benefit, environmental savings, neighboring hospital savings, and health-related economic benefits) of €69.2 million annually, here are approximate yearly net values:
- Average Case Annual Net (Benefits - Costs): €69.2M - €29.5M = €39.7M
- Best Case: 10% higher benefits and 10% lower costs: €76.12M - €26.55M = €49.57M
- Worst Case: 10% lower benefits and 10% higher costs: €62.28M - €32.45M = €29.83M
NPV table (truncated):
| Year | Discount Factor (5%) | Best Case (€) | Average Case (€) | Worst Case (€) |
|---|---|---|---|---|
| 1 | 0.9524 | €49.57M * 0.9524 = €47.25M | €39.7M * 0.9524 = €37.8M | €29.83M * 0.9524 = €28.4M |
| 2 | 0.9070 | €49.57M * 0.9070 = €44.95M | €39.7M * 0.9070 = €36M | €29.83M * 0.9070 = €27.05M |
| 3 | 0.8638 | €49.57M * 0.8638 = €42.8M | €39.7M * 0.8638 = €34.3M | €29.83M * 0.8638 = €25.8M |
| … | … | … | … | … |
| 20 | 0.3769 | €49.57M * 0.3769 = €18.7M | €39.7M * 0.3769 = €15M | €29.83M * 0.3769 = €11.2M |
Summing up all the values for each scenario over the 20-year period yields the following NPV:
- Best Case NPV: €599M - €80M = €519m
- Average Case NPV: €479M - €80M = €399m
- Worst Case NPV: €361M - €80M = €280m
Conclusion:
The establishment of a new hospital in the region addresses a critical healthcare gap while offering numerous direct and indirect benefits. While there are significant costs associated, the multifaceted economic and non-economic returns make a compelling case for its establishment. The Cost Benefit Analysis yields a large benefit in all cases, leaving plenty of space to flex costs and benefits while still achieving a social economic benefit overall.
This report provides a preliminary overview, and a more detailed feasibility study, incorporating more granular data and comprehensive analyses, is recommended to provide a definitive roadmap.
Nevertheless it is to be expected than any further analysis will reach a similarly positive outcome. Therefore the best course of action would be to begin planning as soon as possible and to progress the project as soon as the requisite funding is allocated.
In summation, the provision of a new hospital facility in Ballina, Mayo, holds great promise for the community. By addressing the existing healthcare gap, improving accessibility, and providing a comprehensive range of services, the proposed hospital will significantly enhance the quality of healthcare in the region. With its strong financial viability and numerous benefits to the community, we are confident in the success of this project. We recommend moving forward with the necessary steps to bring this vision to reality, ensuring a brighter and healthier future for the residents of Ballina and its surrounding areas.